What is a flap in dental surgery?
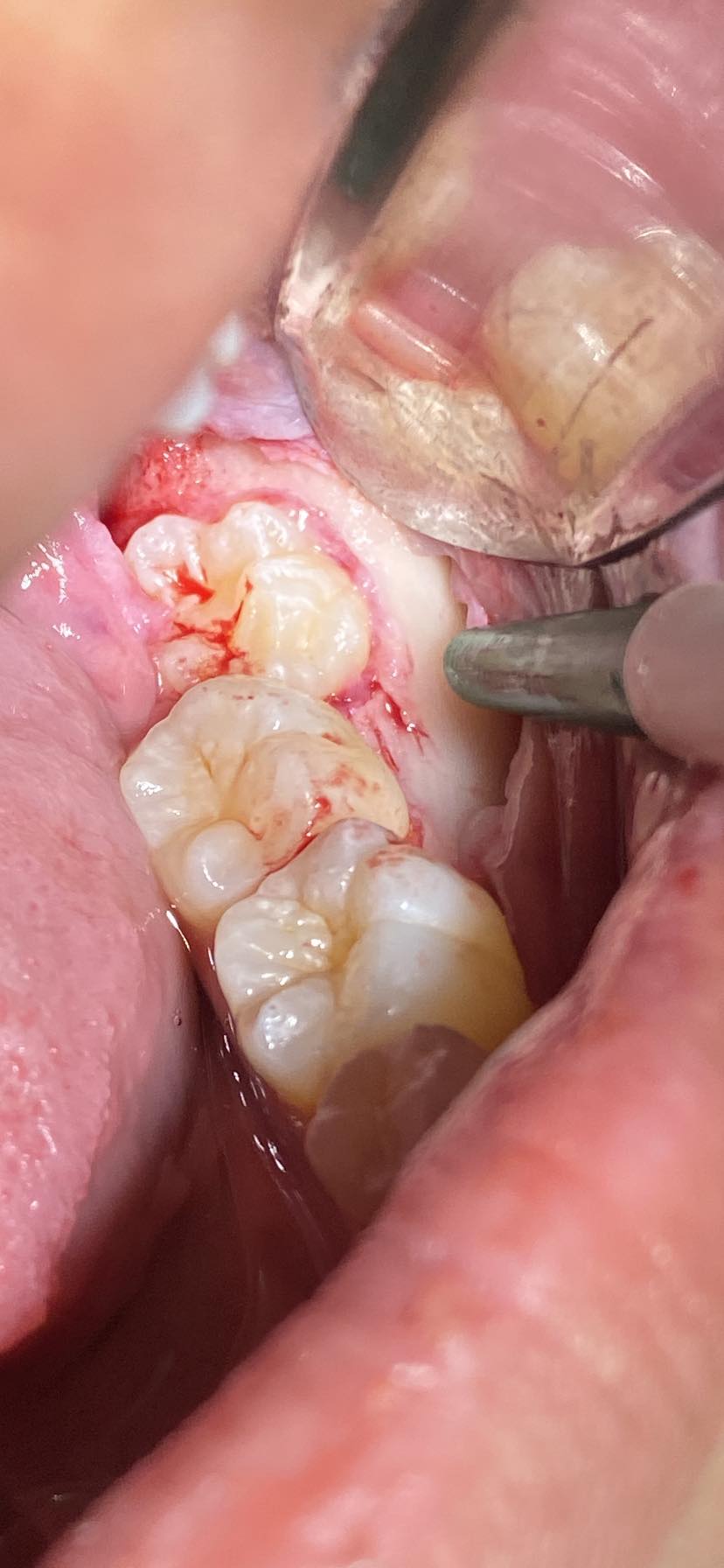
In dentistry, a flap is a portion of soft tissue defined by a surgical incision that retains its own blood supply. It provides surgical access to underlying tissues and can be repositioned to its original location, where it is held in place by sutures and is expected to heal properly.
What is the purpose of a flap procedure?
The main purpose of a flap in dentistry is to access the tooth and bone beneath the mucosa. When performing a routine extraction where a third of the root fractures and needs retrieval, or when extracting multiple teeth, an impacted tooth, or performing an odontectomy, a flap is the technique used.
What are the instruments needed in a flap tray?
In a flap tray for dental surgery, the following instruments are typically needed:
- #15 Blade and Blade Holder: For making precise surgical incisions.
- MPE Molt #9: To severe the periodontal tissues surrounding the tooth that needs to be extracted.
- Elevator/Luxator: To elevate and luxate the tooth from the alveolar socket.
- AdsonTissue Forceps: For grasping and manipulating soft tissues.
- Iris or Mosquito Scissors: For cutting tissues and sutures.
- Minnesota Retractors: To retract or back tissues and provide better visibility and access.
- Seldin Retractors: To retract small soft tissue flap.
- Surgical Curettes: For debriding and cleaning the surgical site.
- Bone Files/Rongeurs: For smoothing and shaping bone.
- Suction Tips: To keep the surgical area clear of blood and fluids.
- Needle Holder: For holding needles while suturing.
- Chromic Gut or Silk Sutures and Needles: This is used to suture or close the flap after the procedure. For ease of use, you can use the swaged needles.
- Gauze Sponges: For absorbing blood and fluids.
- Saline Solution: For irrigation of the surgical site.
What are the principles of dental flap design?
The principles of dental flap design are the following:
- Broad-Based
The outline of the base of the surgical incision should always be broader than the free margins. This is to preserve an adequate blood supply and to prevent ischemic necrosis of the entire flap.
- Sufficient Soft Tissue Reflection
Reflection of the tissue should be adequate (at least 3-4mm) from the incision. This is to provide adequate access for the insertion of instruments required to perform surgery. If there is sufficient soft tissue reflection, you as a clinician could easily hold the flap and retract it without any tension on the soft tissue. Rapid healing can also be expected as long, straight incisions with adequate flap reflection heal more rapidly than a short, torn incision.
- Full Thickness
A flap’s incision should go through and through from the surface mucosa, to the submucosa, up until the periosteum. This is done because the more that the entirety of the soft tissue is intact, the faster the healing process is. Remember that the periosteum is the primary tissue responsible for bone healing, so preserving this portion and replacing it hastens the healing process. A full-thickness flap also lessens bleeding as tissue space between bone and periosteum is avascular.
- Incision over Sound, Intact Bone
Incisions should be made over the intact bone that will be present after the surgical procedure is complete; hence, if you are going to remove the bone, you have to make sure that the incision is made at least 6mm from the remaining bone.
- Incision should Avoid Injury to the Local Vital Structures
The incision should avoid important structures such as the lingual nerve and mental nerve in the mandible to prevent prolonged temporary or permanent paresthesia of the tongue and the greater palatine artery in the maxilla which is located on the posterior lateral aspect of the hard palate that might cause uncontrolled bleeding.
What are the complications of flap design?
Complications in flap design and execution can arise due to various factors. Common complications include:
Flap Necrosis: Inadequate blood supply to the flap, often due to a narrow base or excessive tension, can lead to tissue death.
Dehiscence: This refers to the reopening of the surgical wound, which can occur if the flap is under too much tension, poorly positioned, or if there is infection.
Infection: Poor aseptic technique, inadequate irrigation, or contamination can lead to infection at the surgical site.
Excessive Bleeding: Poor flap design can result in injury to blood vessels, leading to excessive bleeding during and after surgery.
Swelling and Edema: Trauma to tissues can cause significant swelling and edema, complicating healing and patient comfort.
Hematoma Formation: Improper control of bleeding or excessive tissue trauma can result in the collection of blood beneath the flap, forming a hematoma.
Loss of Bone: Flap design that does not adequately protect the underlying bone can result in bone loss, affecting the overall stability and success of the procedure.
Paresthesia: Damage to nerves during flap design or reflection can result in temporary or permanent loss of sensation (paresthesia) in the affected area.
Scarring: Poor flap design and handling can lead to excessive scarring, which might affect the aesthetic and functional outcome.
Delayed Healing: Inappropriate flap design, excessive tension, or infection can delay the healing process.
Flap Retraction: If the flap is not secured properly, it can retract and expose the underlying tissues, leading to complications.
To minimize these complications, careful planning, precise surgical technique, and adherence to the principles of flap design are essential.
What are the flaps used in oral surgery?
Several types of flaps are used in oral surgery, each with specific applications and advantages. The choice of flap depends on the surgical procedure, the location of the surgical site, and the desired outcomes. Commonly used flaps in oral surgery include:
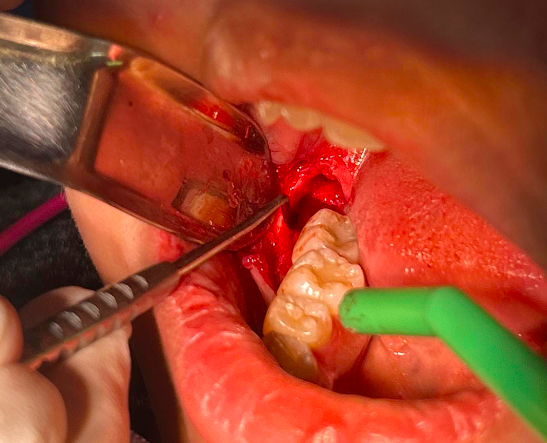
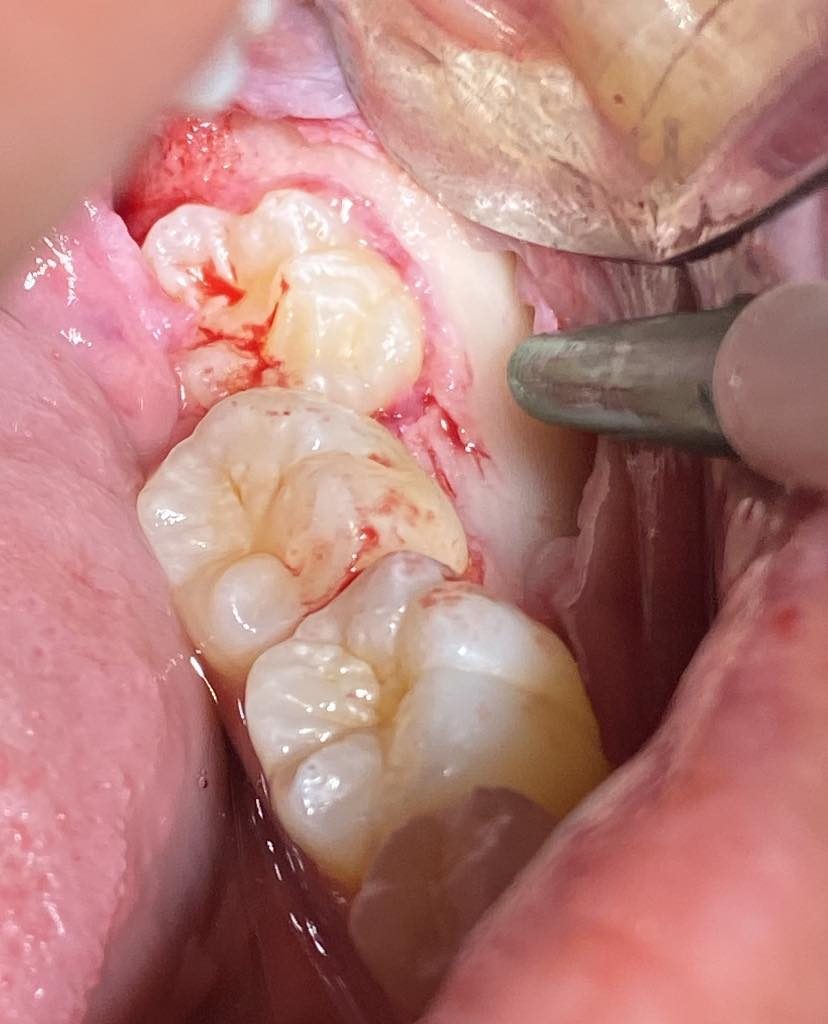
Envelope Flap:
An envelop flap includes a horizontal incision along the gingival margin without vertical releasing incisions.
Indication: Widely used for extractions, minor bone contouring, and implant placement.
Triangular Flap (Three-Cornered Flap):
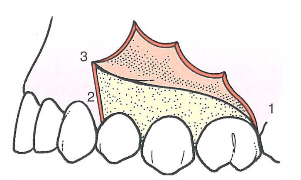
A triangular flap includes a horizontal incision with one vertical releasing incision.
Indication: Provides good access for procedures such as root tip removal or apicoectomy.
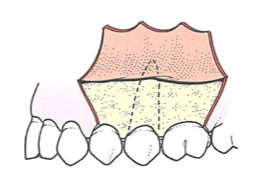
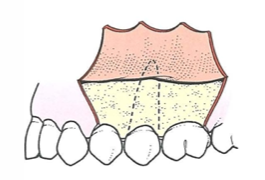
Rectangular Flap (Four-Cornered Flap):
A rectangular flap or a four-cornered flap includes a horizontal incision with two vertical releasing incisions This is the type of flap that allows maximum access and visibility.
Indication: Offers excellent access and visibility for complex surgeries, such as resective periodontal surgery or removal of impacted teeth.
Semilunar Flap:
A semilunar flap is a curved, crescent-shaped incision made apically to the gingival margin; almost at the portion of the apices of the roots.
Indication: This is commonly used for apicoectomy and accessing the periapical area while preserving the marginal gingiva.
Pedicle Flap:
A pedicle flap with a base attached, allowing it to be rotated or repositioned without disrupting its blood supply.
Indication: Commonly used in mucogingival surgery for root coverage procedures or to correct gingival recession.
Papilla Preservation Flap:
A papilla preservation flap is designed to preserve the interdental papilla during periodontal surgery.
Indication: Used in regenerative procedures to maintain esthetics and tissue integrity around the interdental area.
Modified Widman Flap:
A modified windman flap involves internal bevel incisions to remove pocket lining while preserving the outer gingival tissue.
Indication: Primarily for periodontal surgery to reduce pocket depth and remove diseased tissue.
Sulcular Flap (Intrasulcular Flap):
A sulcular flap, as its name suggests, is an incision made within the gingival sulcus, often without vertical releasing incisions.
Indication: Common in regenerative procedures, allowing minimal disruption to the gingival margin.
Edentulous Flap:
An edentulous flap is specifically designed for edentulous areas with horizontal and/or vertical incisions. The incision is usually done at the center of the residual ridges as this portion of the gingiva is devoid of vital anatomical structures that could cause damage when severed.
Indication: Useful for ridge augmentation, alveoloplasty, and implant placement in edentulous regions.
Free Gingival Graft:
A free gingival graft is done when a tissue is harvested from a donor site (often the palate) and transplanted to another site.
Indication: Used to increase the width of attached gingiva or cover exposed roots.
Each type of flap is tailored to provide optimal access and visibility for the specific surgical procedure while minimizing trauma and promoting healing.
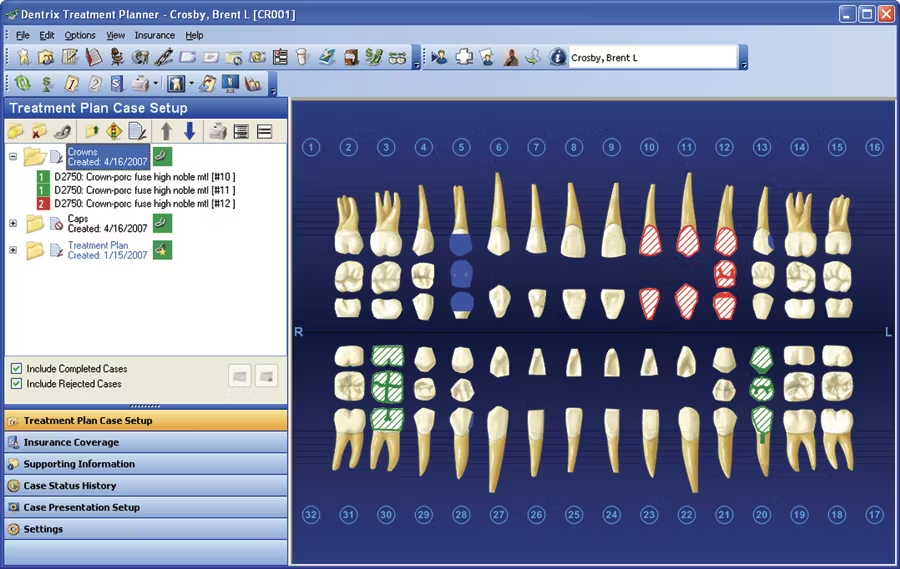
Flap surgery dental cost
The cost of flap surgery in dentistry can vary widely based on several factors, including geographic location, the complexity of the procedure, the specific dental practice, and whether the surgery is performed by a general dentist or a specialist such as a periodontist. Here is a general overview of potential costs:
Basic Flap Surgery:
Cost Range: $200 to $600 per quadrant.
Details: This can include scaling and root planing along with the surgical flap procedure to treat periodontal disease.
Complex Flap Surgery:
Cost Range: $500 to $1,500 per quadrant.
Details: More extensive procedures, such as those involving bone grafts, membrane placement, or guided tissue regeneration, can be more costly.
Gingival Grafting:
Cost Range: $600 to $1,200 per site.
Details: This includes procedures where tissue is taken from another part of the mouth (usually the palate) and grafted onto the surgical site.
Periodontal Flap Surgery:
Cost Range: $1,000 to $3,000 for full-mouth surgery.
Details: For patients requiring extensive treatment across multiple quadrants, the cost can accumulate.
Insurance Coverage:
Many dental insurance plans cover a portion of periodontal flap surgery costs, especially if the procedure is deemed medically necessary. Patients are often responsible for a copayment or a percentage of the total cost.
Consultation and Diagnostic Fees:
Cost Range: $50 to $200.
Details: Initial consultation, examination, and any necessary diagnostic imaging (such as X-rays) are additional costs to consider.
Patients are advised to check with their dental insurance provider to understand the extent of coverage and out-of-pocket expenses. Consulting with a dental professional can provide a more accurate estimate based on individual needs and the specific details of the required surgical procedure.



Great write-up, I am regular visitor of one¦s web site, maintain up the excellent operate, and It is going to be a regular visitor for a long time.